
Pelvic Health and Back Pain: The Overlooked Connection
That nagging lower back pain might not be "just your back." Your pelvic floor is part of your deep core system, and when it's weak or dysfunctional, your spine loses...

Before proceeding toward an accurate diagnosis, it is crucial to establish a patient’s history. This is done during the appointment with a doctor. The patient must be as truthful as possible during the process. The nurse or doctor may ask the following questions:
The tests conducted to diagnose the condition can be carried out through imaging or physical examination like intrarectal and vaginal exams. However, if the patient does not want a physical exam, they can opt for any of the three procedures listed below:
Your pelvic floor is a small group of muscles with a big job: it supports your organs, helps control your bladder and bowel, contributes to sexual function, and works as part of your deep core. When these muscles are coordinated—able to contract and relax—you feel more supported in everyday life: lifting, laughing, running, sneezing, and recovering after pregnancy. This guide explains what the pelvic floor is, how it works, and a safe way to start training—no gimmicks, just gentle, consistent practice.
Medically reviewed by Wanda Cotie, PT, DPT — Last reviewed: [Date]
The pelvic floor is a sling of muscles and connective tissue at the base of your pelvis. It supports your bladder, uterus, and bowel; helps maintain continence; and coordinates with your diaphragm and deep core to manage pressure when you breathe, lift, or move.
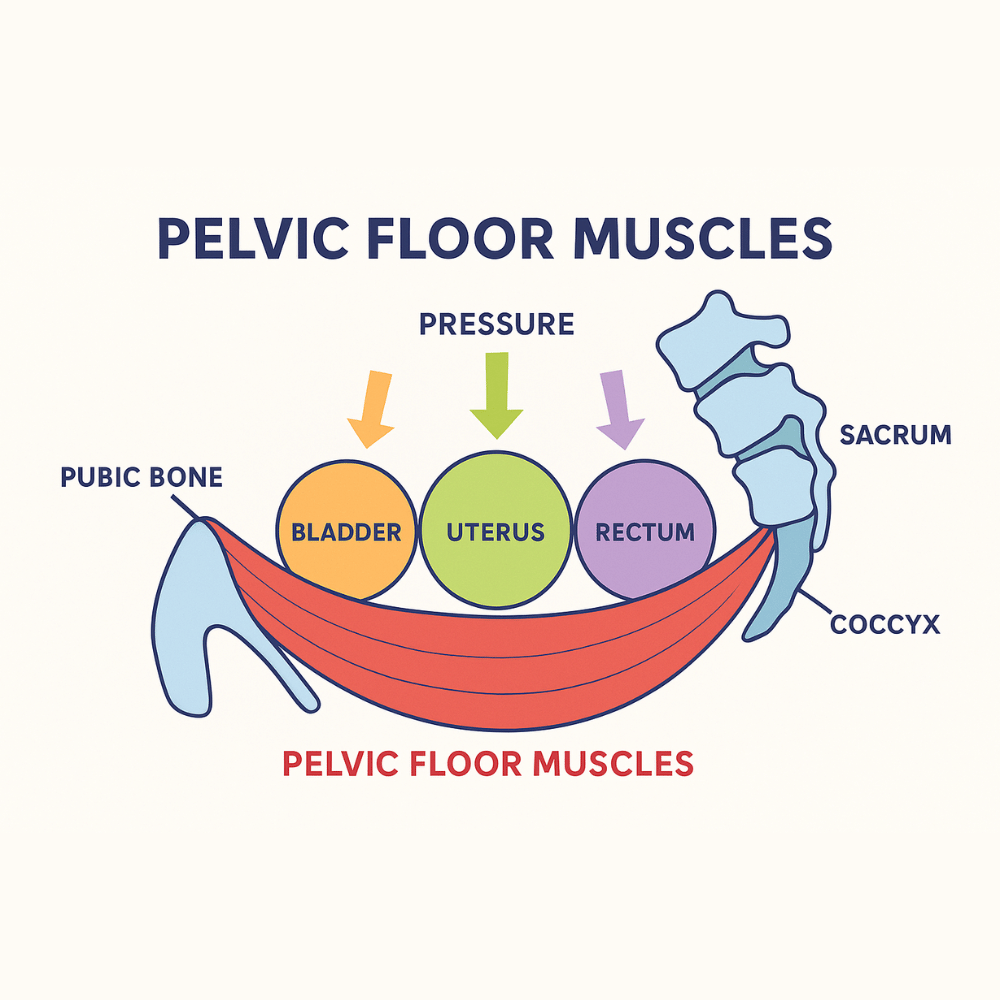
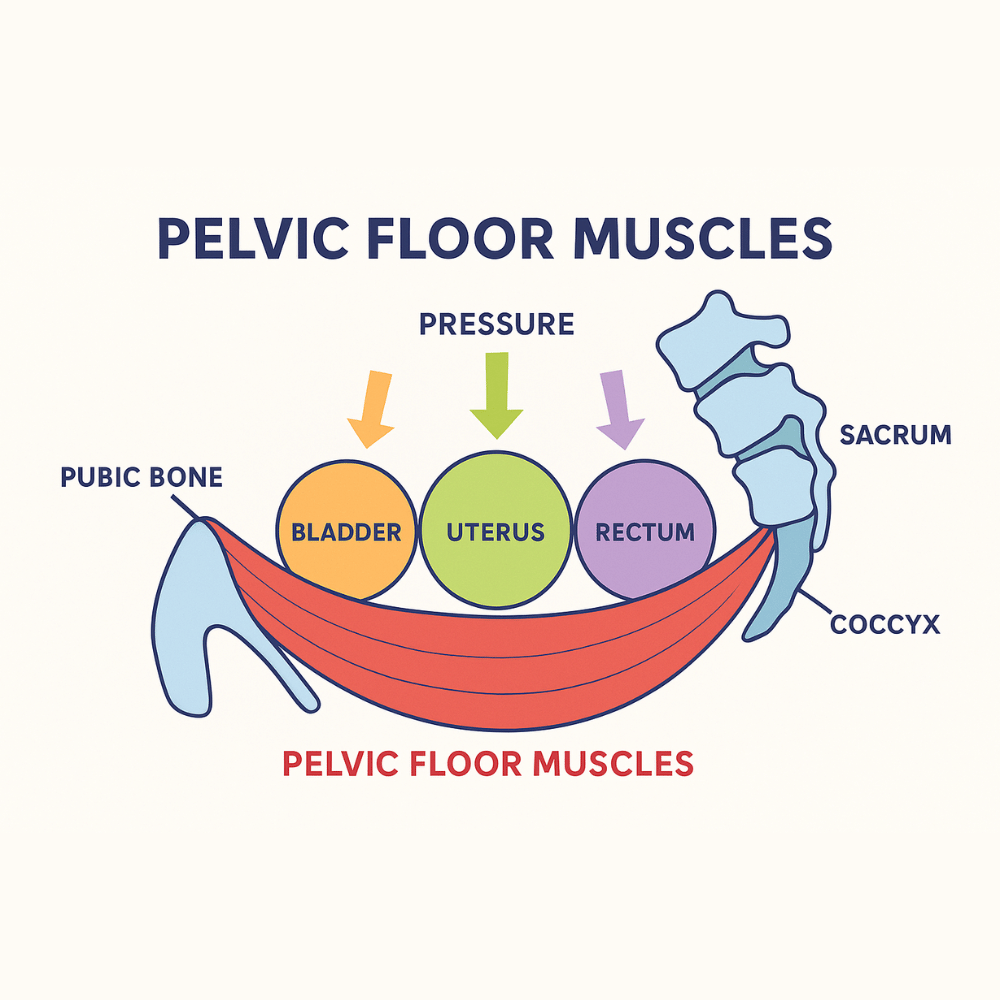
Your pelvic floor is a group of muscles forming a supportive hammock at the base of your pelvis. These muscles hold up the bladder, uterus, and rectum while helping with core stability, posture, and continence. A strong pelvic floor supports everyday movement, sexual health, and recovery through life stages like pregnancy and menopause.
Think of the pelvic floor like a soft, flexible hammock. It attaches from your pubic bone to your tailbone and across the sit bones. These muscles:
You’ll sometimes hear clinicians talk about layers—superficial, middle, and deep. The takeaway isn’t to memorize anatomy, but to understand that good training reaches more than one layer and teaches timing and relaxation too (not just “squeeze harder”).
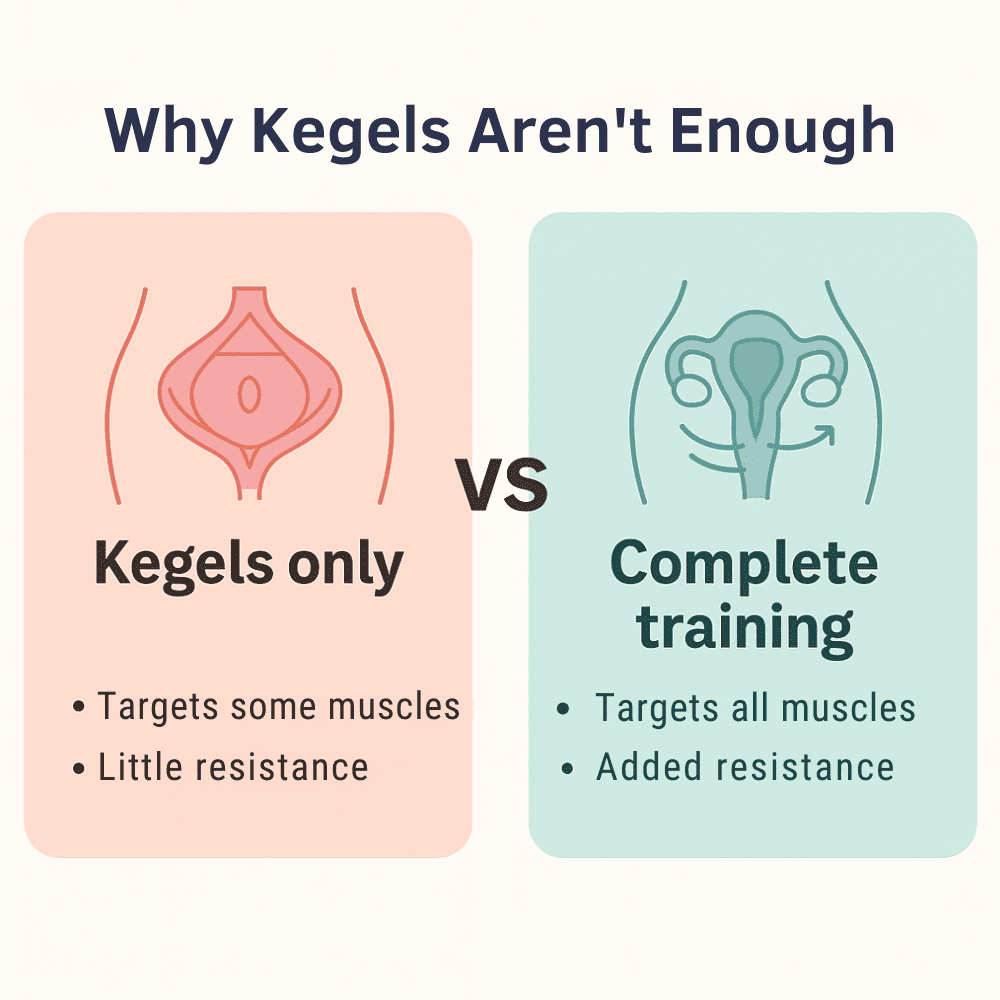
Kegels are a contraction. Training is a plan. Strong, reliable pelvic floors need strength, endurance, coordination, and the ability to relax. Common pitfalls include bearing down instead of lifting, holding your breath, or doing too much, too soon. Adding gentle resistance can help your brain “find” the right muscles, improve awareness, and make progress feel more tangible—similar to how a light band makes a glute bridge easier to perform correctly.
Start 3–4 days per week. Find a calm minute. Breathe. No rushing.
1) Breath priming — 1 minute
2) Foundational contractions — 3 sets × 10
3) Endurance holds — 2 rounds
4) Release & reset — 1 minute
Safety first: Stop if you feel sharp pain, burning, fever, or new symptoms such as bulging/heaviness that worsens. Seek guidance from a pelvic floor physical therapist or your OB-GYN if you’re unsure where to start, recently gave birth, or have a diagnosed condition (e.g., prolapse, persistent pain).
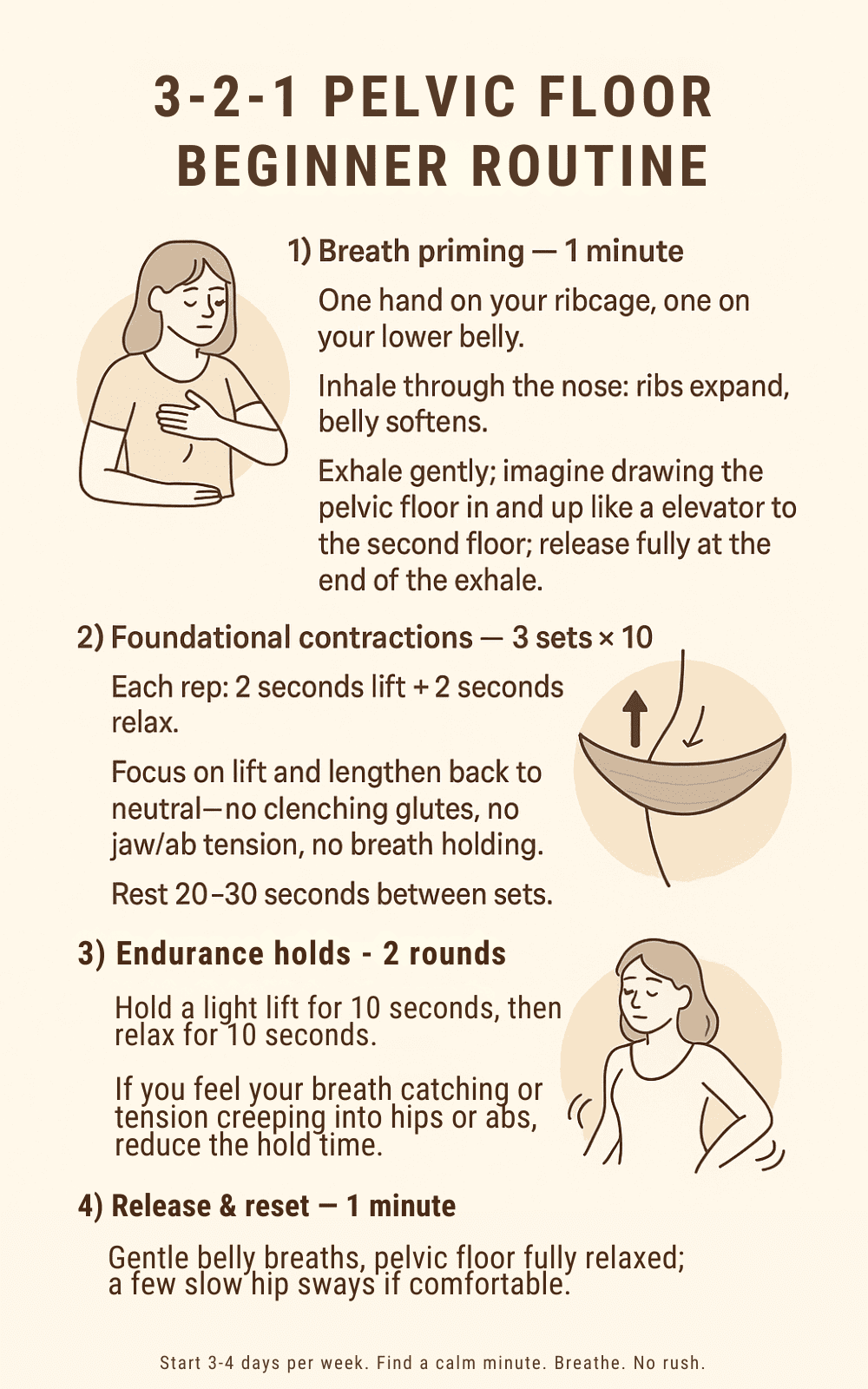
Build strength and awareness in just a few minutes a day. The 3-2-1 routine combines breath, gentle contractions, endurance holds, and release work to train all layers of your pelvic floor. Follow along with this visual guide for a clear, easy-to-remember practice you can do anywhere.
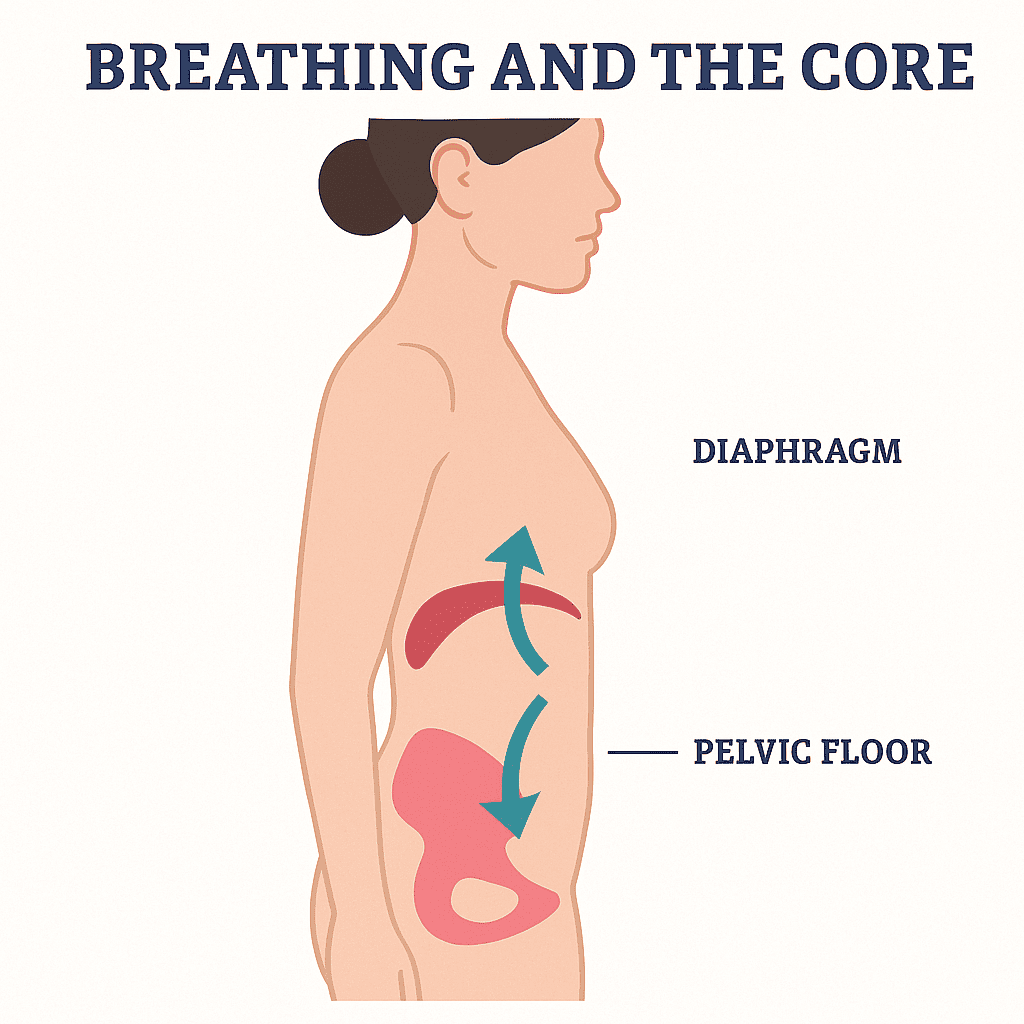
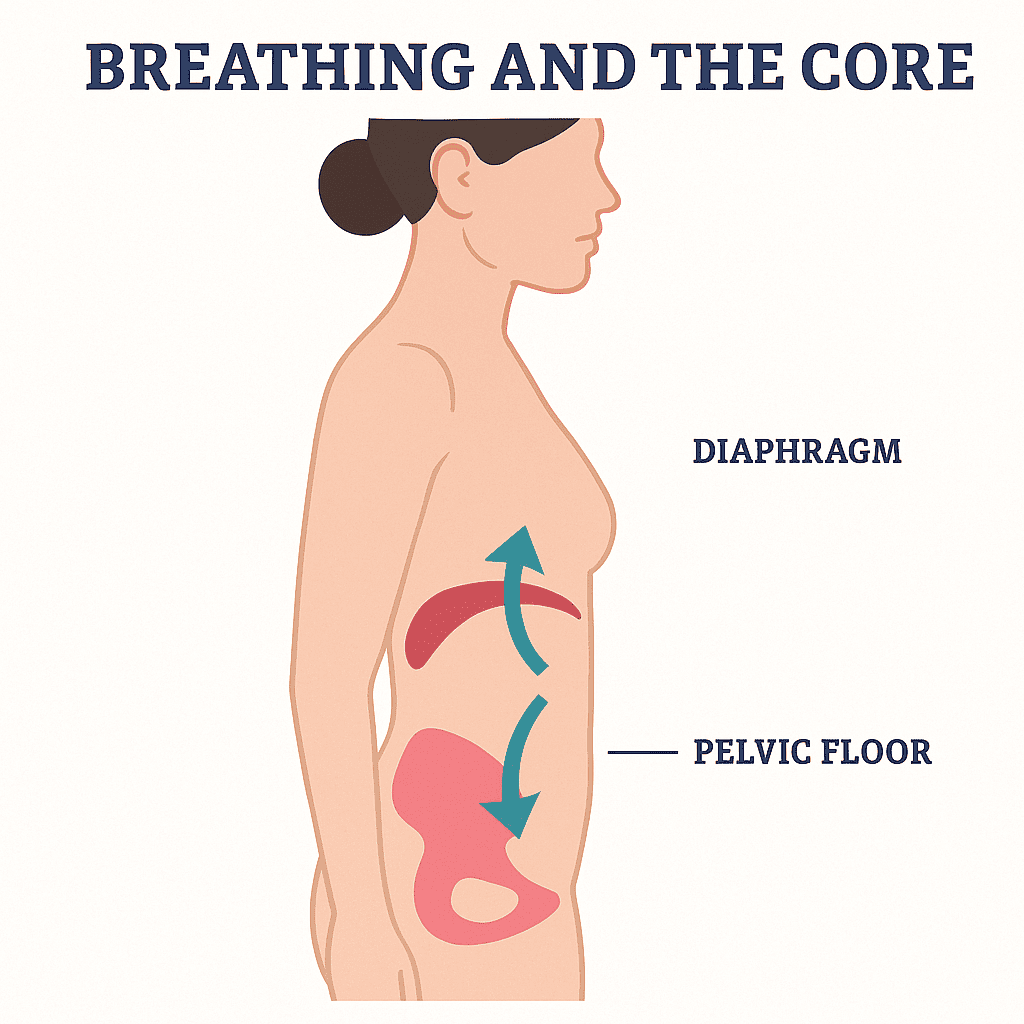
Your pelvic floor and diaphragm are dance partners. When you inhale, the diaphragm descends and the pelvic floor responds; when you exhale, a gentle lift becomes easier. Stack your ribs over your pelvis (not a military brace, just tall and easy). For daily life:
Strong pelvic floor muscles support you in the moments that matter — from carrying groceries and enjoying a jog to playing with your kids. Training these muscles helps improve stability, continence, and daily confidence, so you can move freely and live fully.
Keep it simple: a two-minute journal after sessions noting date, sets, holds, and how things felt (easy/ok/challenging). Add real-life markers—fewer leaks with sneezing, better control during workouts, and improved comfort. Progression ideas:
Many people find that light, body-safe resistance improves awareness and consistency. That doesn’t mean “more is better”—it means better feedback is better. If you explore tools, look for:
Femme Flexor checks those boxes with platinum-grade silicone, a patented (patent-pending in some listings) design intended to engage the pelvic floor’s tissue layers, and an easy, non-electronic approach you can use at home—crafted in Canada with clinician input.
Book with a pelvic floor physical therapist or speak with your OB-GYN if you notice persistent leaking, heaviness/bulge sensations, pain with penetration, or if symptoms limit your daily activities. An expert eye can tailor cues, positions, and progressions so training feels effective—not confusing.


Designed with patented innovation and 100% body-safe silicone, the Femme Flexor helps you go beyond basic Kegels. Its gentle resistance strengthens all three layers of the pelvic floor, building lasting strength and support for everyday life. Simple, discreet, and backed by science.
Femme Flexor’s approach is intentionally simple, science-led, and non-tech. No beeps or endless charging—just a thoughtfully designed, platinum-grade silicone tool that adds gentle resistance so your routine feels doable anytime, anywhere. That’s the heart of long-term success: practical, repeatable habits supported by smart design.
It supports your pelvic organs, helps control bladder and bowel function, contributes to sexual function, and works with your diaphragm and deep core to manage pressure during movement.
Kegels are a contraction. Training is a plan that builds strength, endurance, coordination, and relaxation—often with breath work and, for some, gentle resistance to improve awareness.
Start with 3–4 sessions per week using the 3–2–1 routine (breath, contractions, endurance holds, release). Consistency beats intensity.
No. Many people succeed with body-weight awareness and breath. Some prefer a simple, body-safe resistance tool for better feedback and adherence—Femme Flexor is designed for exactly that, without electronics.
Use only products made from body-safe materials and follow cleaning instructions. Stop if you feel pain and consult a clinician for personalized guidance.
Everyone’s timeline varies. Many notice improved awareness and control within weeks when they train consistently and breathe well.
Postpartum training is beneficial with appropriate progression; pregnancy requires clinician guidance—especially regarding penetrative tools. If you’re pregnant, only use a tool if your provider confirms it’s safe for you.
Femme Flexor was designed with a sexual-wellness experts Wanda Cotie and het daughter Madeline Dorion and pelvic floor physiotherapist, and it’s proudly made and patented in Canada.
100% body-safe platinum-grade silicone with a patented design that provides gentle resistance to support training.
If you experience persistent leaking, heaviness/bulging, pain, bleeding, fever, or symptoms that limit your daily life, get a personalized assessment before continuing.
What’s been missing from your workout all these years.

That nagging lower back pain might not be "just your back." Your pelvic floor is part of your deep core system, and when it's weak or dysfunctional, your spine loses...

Ready to start training with your FemmeFlexor? This beginner-friendly guide walks you through every step; from preparing your space and comfortable insertion to building a progressive routine. Learn proper technique,...

Bladder leaks when you laugh? Pelvic heaviness by day's end? These common signs mean your pelvic floor is asking for help. Learn what the 5 key symptoms actually mean, when...